This article is part of the Debatable newsletter. You can sign up here to receive it on Tuesdays and Thursdays.
More than two years after the coronavirus emerged, and more than a year after the first vaccines for it arrived, suffice it to say that the light at the end of the pandemic tunnel appears dimmer than one might have hoped.
As the stunningly infectious Omicron variant sweeps the country, case rates have blasted past all previous peaks; hospitalizations, too, have now broken last winter’s record. The surge has threatened another round of school closures and stifled the economy as working parents struggle to care for their children, who themselves are finding their lives upended once again.
Omicron cases are likely to peak nationally during January in “an intense month of disruption,” according to projections from Jeffrey Shaman, an infectious disease modeler and epidemiologist at Columbia. So how should the Biden administration, businesses, schools and the rest of the public respond? Here’s what people are saying.
Three ways of dealing with Omicron
Broadly speaking, there are three approaches the United States could take to the current surge, as Leana Wen, a visiting professor at George Washington University Milken Institute School of Public Health, writes in The Washington Post.
The first option is to impose lockdowns to flatten the curve of infections, as the Netherlands, Austria and parts of China have done, perhaps combined with another round of social spending to help Americans weather the disruption. But the public seems largely opposed to the idea of business closures, as does the Biden administration. “We are not going to write checks to incentivize people to sit at home, and we are not going to bail out businesses if the economy seems strong,” a senior White House official told CNN.
The second option is to let the virus run its course by lifting most or all nonpharmaceutical interventions. After all, a majority of Americans are vaccinated, and preliminary evidence does suggest that Omicron causes milder illness than previous variants. Why not treat it like the flu?
[“Why More Americans Are Saying They’re ‘Vaxxed and Done’”]
The principal objection to this laissez-faire approach is that it could cripple the health care system. According to one model that tracks hospital capacity nationwide, seven states — including California and Texas — are expected to exceed their hospital capacity in the next 10 days.
From the perspective of Craig Spencer, an emergency room doctor in New York City, the Omicron surge is not like the first Covid wave of March 2020: With vaccines, treatments and a seemingly less lethal variant, fewer of his patients now need life support. Yet the sheer number of infections has produced a rapid influx of patients, as well as record levels of employee infections and staff shortages.
“Fewer providers means fewer available beds because there are only so many patients a team can treat at a time,” he writes. “This also means treatment is slower and people will spend more time in the E.R. And the longer these patients stay in the E.R., the longer others remain in the waiting room. The domino effect will affect all levels of the health care system, from short-staffed nursing homes to ambulances taking longer to respond to 911 calls.”
[“Hospitals Are in Serious Trouble”]
The third option is to pick a middle path, one that aims to save the hospital system from being overwhelmed while minimizing public disruption.
In Wen’s view, this approach would entail boosting all nursing home residents and staff; mandating proof of vaccination and boosters for indoor dining, gyms, movie theaters and sporting events; requiring high-quality masks in all indoor public spaces; and expediting vaccine approval for children under 5.
To increase vaccine uptake, Anthony Fauci, the nation’s top infectious disease expert, recommended that the federal government seriously consider a vaccine mandate for domestic air travel.
At the same time, to alleviate staff shortages, Wen suggests that the Centers for Disease Control could reduce or even waive isolation and quarantine requirements for people working in critical jobs while still mandating high-quality masks.
What about schools?
Perhaps no other question about the proper policy response to the Omicron surge has bred so much contention and confusion.
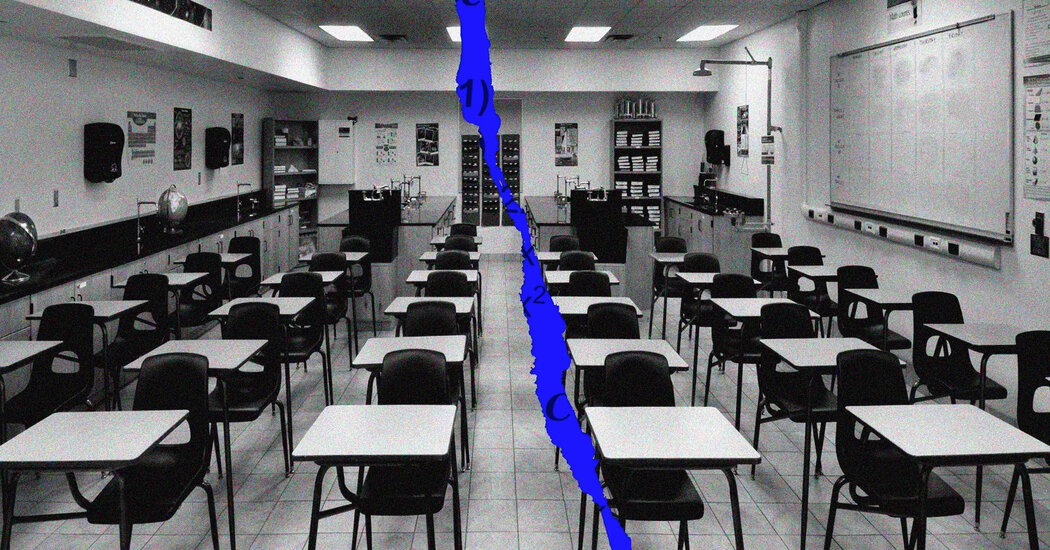
There is widespread acknowledgment, as Joseph G. Allen notes in The Times, that the harms children have suffered from being out of school are severe, cumulative and potentially long-lasting, the most obvious among them being learning loss.
But education is just one of many vital public goods Americans rely on schools to provide. They are also a source of child care, food security, socialization, and domestic violence prevention. For all these reasons, Allen argues, “a new round of widespread school closures would be a tragic mistake and should be off the table as an option.”
Yet keeping schools open during the Omicron surge is a question not just of values but of possibility. As The Times’s Dana Goldstein has reported, schools across the country are facing test kit and staffing shortages, forcing many to switch to remote instruction. Many of the nation’s largest school systems, including New York City’s, have vowed to keep students in classrooms. But it’s not clear how much learning can occur under current epidemiological conditions.
Other countries have shown that keeping schools open is possible with sufficient political will. Britain, Stephanie H. Murray points out in The Atlantic, is determined “to ask as little as possible of children,” imposing harsher restrictions on adults so that students can continue to go to school. “Even during the strictest portion of last year’s lockdown, when all pubs and restaurants were closed and sitting on a bench with someone you ran into at the park was illegal, in-person schooling remained available for vulnerable kids and children of essential workers,” she writes.
Americans, by contrast, “have accepted more harm to children in exchange for less harm to adults, often without acknowledging the dilemma or assessing which decisions lead to less overall harm,” The Times’s David Leonhardt writes. “Given the choices that the country has made, it should not be surprising that children are suffering so much.”
Getting to a ‘new normal,’ for Omicron and beyond
Beyond January, the virus’s trajectory is uncertain. “The future burden of Covid depends in large part on whether highly transmissible variants able to evade pre-existing immunity, such as Omicron, continue to emerge,” Jeffrey Shaman writes. “If new variants arise roughly twice per year, for example, then we should expect multiple outbreaks each year, even in the summer.”
The Biden administration’s response to Omicron does not bode well for that eventuality, the Times columnist Zeynep Tufekci argues. It was, after all, just a matter of luck that Omicron seems to cause less severe illness. “If it had been more deadly — as Delta has been — the U.S. government’s haphazard and disorganized response would have put the whole country much more at risk,” she writes. “Even with this more moderate threat, the highest-ranking public health officials are making statements that seem more aimed at covering up or making excuses for ongoing failures, rather than leveling with the public.”
So what would a more future-proof public health approach look like? Last week, six former advisers to the Biden administration who were frustrated with its coronavirus response took the unusual step of publicly calling for a new domestic pandemic strategy. In three Journal of the American Medical Association articles, the authors write that the country must shift to a “new normal” in which the coronavirus does not disappear but instead circulates alongside other respiratory viruses like the flu.
Getting to the “new normal” they envision would require not concession but aggressive adaptation:
-
First, because interventions to reduce coronavirus transmission, like ventilation, work across respiratory pathogens, the authors argue that public health decisions should from now on be based on the aggregate risk of all respiratory viruses. Policymakers then need to establish an aggregate risk threshold beyond which emergency measures would be triggered. In their view, the appropriate threshold would reflect the peak weekly deaths, hospitalizations and transmission of viral respiratory illnesses during prepandemic, high-severity years. (In the worst week of 2017-18, for example, about 3,000 Americans died of respiratory viruses.)
-
Second, to ensure that total respiratory viral infections, hospitalizations and deaths do not exceed severe prepandemic levels, the authors call for a vaccine coverage rate of at least 90 percent (which will require vaccine mandates); development of mucosal, variant-specific and universal coronavirus vaccines; and rapid production of therapeutics, along with a mechanism to make them immediately and freely available to anyone who tests positive.
-
Third, to reduce Covid transmission and sustain the “new normal,” the authors argue the nation would need a greatly improved public health infrastructure that includes a new, permanently funded system for testing, surveillance and mitigation measures.
“Without a strategic plan for the ‘new normal’ with endemic Covid-19, more people in the United States will unnecessarily experience morbidity and mortality, health inequities will widen, and trillions will be lost from the U.S. economy,” they write. “This time, the nation must learn and prepare effectively for the future.”
Do you have a point of view we missed? Email us at debatable@nytimes.com. Please note your name, age and location in your response, which may be included in the next newsletter.
READ MORE
“America’s Covid Rules Are a Dumpster Fire” [The Atlantic]
“Europeans Ponder Living With, Not Defeating, Covid” [The New York Times]
“Here’s Why You’re Wrong for Supporting Either In-Person or Virtual School” [McSweeney’s]
“Disruption, Dismay, Dissent: Americans Grapple With Omicron’s Rise” [The New York Times]
“Covid is here to stay: countries must decide how to adapt” [Nature]