A significant proportion of healthcare in Myanmar is now being delivered outside state hospitals, by doctors and nurses who oppose the military and are loyal to the National Unity Government challenging the junta’s legitimacy, medical workers in the country told the BBC.
Most interviewees’ names have been changed for their security.
Organised resistance to the 1 February coup in Myanmar started with healthcare workers announcing a boycott of state-run hospitals. They led the first street protests, calling it the “white coat revolution”.
That put medics on a collision course with the junta, and has resulted in much of Myanmar’s healthcare system going underground.
In many areas more than 70% of health workers are believed to have abandoned their jobs, their hospitals and their patients. It was a difficult ethical decision, one defended by senior doctors in a letter they sent to the medical journal The Lancet.
“Our duty as doctors is to prioritise care for our patients – but how can we do this under an unlawful, undemocratic, and oppressive military system?
“Fifty years of previous military rule failed to develop our health system and instead enshrined poverty, inequality, and inadequate medical care. We cannot return to this situation.”
Grace, a teacher at the Yangon Nursing University, says they all “chose to join the CDM [civil disobedience movement]”.

“Every evening at 8pm, we would bang on pots and sing the revolutionaries’ songs in front of the school. We were enraged – how could they just arrest our leader after they had lost an election?”
Grace was one of thousands of medical personnel who not only left her job – losing her accommodation as a result – but also joined the protests to help the injured.
“We arranged ambulances in case someone was shot. Our biggest concern was how to move them to safe areas.
“For minor injuries we would take them to the ambulance and treat them there. For gunshot wounds, we had to find safe routes to the clinics we set up in temples and monastery compounds.”
From these desperate, improvised beginnings they built a shadow health system, notionally under the authority of the National Unity Government (NUG) which was declared in April by ousted parliamentarians to challenge the junta’s authority.
In reality though, the system is run by thousands of volunteers across the country, working in charity clinics or those private hospitals willing to risk having them, and using encrypted communication apps to avoid detection.
They are providing healthcare that is either no longer available in the thinly-staffed state hospitals, or not wanted by patients who oppose the coup.

Dr Zaw Wai Soe, an orthopaedic surgeon and a leading figure in the ousted government’s fight against Covid-19, is the NUG’s health minister.
After the coup he turned down an offer from the military to be their deputy health minister, and went into hiding. He has been charged by the military authorities with treason.
The NUG raises money from Burmese living overseas to support the volunteers, and has set up a Facebook page for patients to get online medical advice from doctors who are in hiding – so-called telemedicine.
“We don’t have enough money,” Zaw Wai Soe told me, speaking from an undisclosed location. “But we do have support from local people, and internationally from the diaspora. It isn’t enough but we are trying as hard as we can to provide proper healthcare.”
A dangerous job
But working underground, in defiance of the military, is dangerous.
The World Health Organisation noted that, by July, half of the 500 attacks on health workers it recorded around the world had occurred in Myanmar.
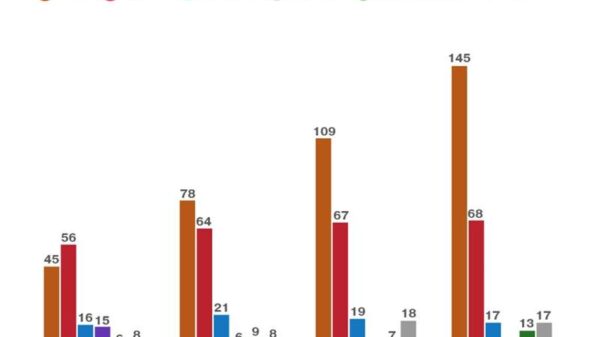
A similar project at Manchester University reported that in the same period 25 medical workers had been killed in Myanmar, 190 arrested, and 55 hospitals occupied by the military.

Luke was an ICU nurse in a private hospital in Mandalay. He says he left his job immediately after the coup, because the hospital’s owner had close ties to the armed forces, and became a protest leader.
“They arrested me on 5 April and took me to Mandalay Palace (where the city’s military command is based). They had promised not to harm us, but once we were in the palace they started beating and questioning us.
“Then they sent us to Obo prison. We were kept in one room, 50 of us. We all had to share a single toilet, and could wash only once a day. It was summer, the hottest time of year, and there was not enough drinking water.”
Luke was kept in prison for 87 days, before being released in an amnesty. These days he is working in a mobile operating theatre in Mandalay hidden inside a shipping container.
“The lighting is not very good. But we do what we can. In prison I saw some gunshot wounds that had not been treated properly in government hospitals. Some died from those wounds.
“Those hospitals do have better equipment, but not enough skilled specialists and nurses. They often don’t accept patients in need of critical care. I think our medical care is better, because we have more specialists than them. Our main problem is that we cannot work openly.”
Some nurses described to me working in hidden charity clinics in Yangon and Mandalay, which are disguised as Covid testing centres to avoid military raids. Most have moved home several times already fearing arrest.
When they leave to go to work, they wear ordinary clothes, not uniforms, and leave their mobile phones behind, in case they are detained. They must always take care to avoid traps set by the military – several medics have been arrested this way.
“We have to be alert when we get called to a patient’s house”, says Nway Oo, a nurse who has gone back from Yangon to her home town in Shan State. “We check with our people in that area to confirm whether the patient is really sick. So, we always wait for a day to be sure the patient is genuine.”
Another nurse I spoke to said she has not left her home in Yangon for five months, and lives in fear of the security forces doing house inspections in her street.
Coping with Covid
Relying heavily on telemedicine, the underground health system has also struggled to treat patients during a surge in Covid infections in July and August.
Myanmar had begun a promising vaccine programme before the coup, but that came to a halt after the military seized power. One of those they arrested was the doctor in charge of the vaccine rollout.
The junta has promised to speed up vaccination rates, but been held back by a lack of trained staff, a lack of vaccines, and a lack of public trust in the military-run health system. The NUG launched its own vaccine programme in July, but this has been largely limited to border areas under the control of sympathetic ethnic insurgent armies.

“It is heartbreaking,” says Mi April, a nursing instructor who is helping her former students to treat patients in their hometowns through telemedicine.
“I used to work until 1 or 2am responding to all the messages I got from people with sick family members, saying my father will die, my mother will die, please respond.
“I was helpless because I could not give them oxygen or medicines. People were queuing at places supplying oxygen, but the military was blocking them from accessing it.”
The Delta variant of Covid appears to have run unheeded through Myanmar in July and August. Real casualty numbers are hard to know. All the nurses and doctors we spoke to say seriously ill patients were turned away from government hospitals, and had to go home, either to recover, or die.
By September Covid numbers had fallen sharply, but Myanmar remains vulnerable to future outbreaks, with vaccination rates still far below neighbouring countries.
“During the worst Covid outbreak this year, we tried to obtain medicines, oxygen concentrators, cylinders, and other equipment. It is a very difficult situation, but we do have manpower, because I believe 70 to 80% of healthcare workers are working with us,” Zaw Wai Soe told me.
‘We lost our future’
I asked him why health workers in Myanmar were playing such a large role in opposition to the coup. He believes it is a moral response by a profession which was terribly neglected during the previous period of military rule, when Myanmar had one of the world’s lowest levels of healthcare spending.
That only started to change under the civilian government led by Aung San Suu Kyi, with a huge recruitment drive to bring in new staff.
“If you compare with other countries, we don’t get big salaries. Most of us could easily go and earn more working in other countries, like Malaysia, Singapore and Brunei. But, especially after Covid arrived last year, we gave all of our efforts to the country. We all expected we would have a better future one day, with our elected government.
“Then suddenly this coup happened. That is why we could not accept this. We were working for the people, even with our poor salaries and living standards.
“We had hopes for the future, and suddenly we lost that future.”
This video can not be played