The current spike in coronavirus cases appears to be less deadly than earlier waves, but some safety-net hospitals are still being severely strained.
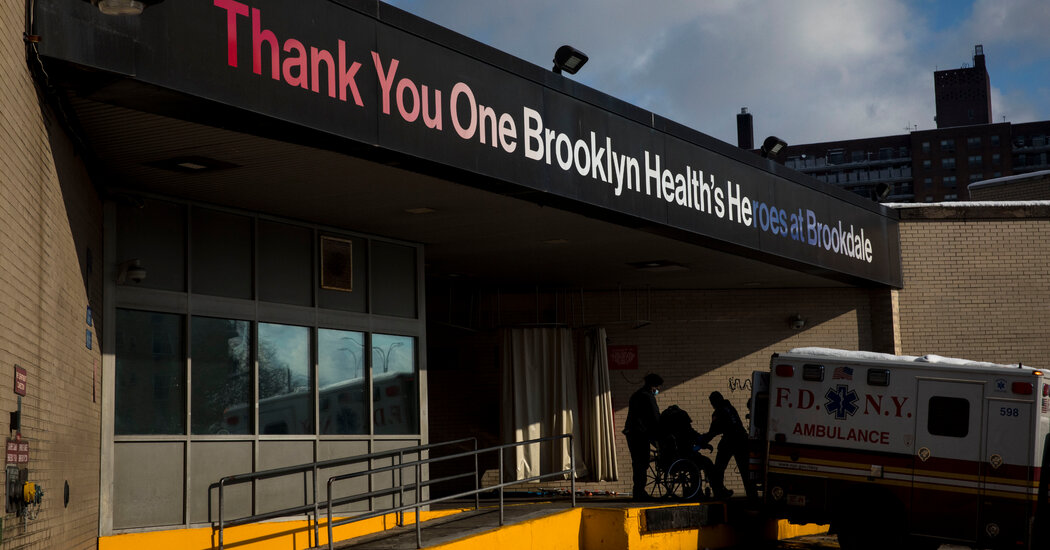
At Interfaith Medical Center in Brooklyn, the intensive care unit is full, mainly with Covid patients. In a scene reminiscent of spring 2020, patient beds have been set up in the hallway.
But on Wednesday, when Interfaith asked city officials to divert ambulances to other hospitals, the request was granted for only two hours, the hospital’s top executive said. Emergency rooms at neighboring hospitals were also overflowing, or precariously understaffed.
“All hospitals, not just safety net hospitals, in Brooklyn and in other boroughs are stressed,” the executive, LaRay Brown, said. Ms. Brown is the chief executive at One Brooklyn Health, which runs Interfaith and nearby Brookdale Hospital.
As the Omicron variant of the coronavirus sweeps through New York, many hospitals are being pushed to their limits by twin challenges: spiking numbers of virus cases and growing shortages of nurses, doctors and technicians. Many workers are sick with Covid-19; others who quit amid the pandemic have not been replaced.
While the latest virus wave appears to be less deadly than earlier ones, with many fewer patients on ventilators, even large hospitals with empty intensive care beds are straining to handle the surge in caseloads because so many workers are out, health care officials said.
“I think everyone across the region is struggling,” said John D’Angelo, who oversees the emergency departments at Northwell Health, the state’s largest health system. Because of its own staff shortages, Northwell has had to limit the number of patients it can take from Interfaith and other beleaguered hospitals.
Almost 4,000 Northwell employees, or 5 percent, were out as a result of Covid-19 on Thursday, Dr. D’Angelo said. That was about double the number at the height of the first virus wave. The system can transfer employees between hospitals as needed, but its emergency rooms have been operating at up to twice their normal volume and waiting times are up. Dr. D’Angelo likened the daily effort to keep positions filled to a game of “whac-a-mole.”
For smaller community hospitals with fewer resources, the situation is more critical. At Interfaith and Brookdale and their affiliated nursing homes, 471 out of 7,000 staff members were out with Covid-19 this week, forcing some nurses to handle double the usual number of patients, Ms. Brown said.
“It is challenging for the hospitals, but it is particularly stressful for our safety net institutions,” said Kenneth E. Raske, the president of the Greater New York Hospital Association, a trade group. “A number of them have requested assistance, including staffing assistance from the state. The problem is the cupboard is bare.”
Similar situations are playing out around the country, including in New Jersey, where officials are working with the federal government and the National Guard to deploy medical teams to hospitals that are experiencing severe staff shortages.
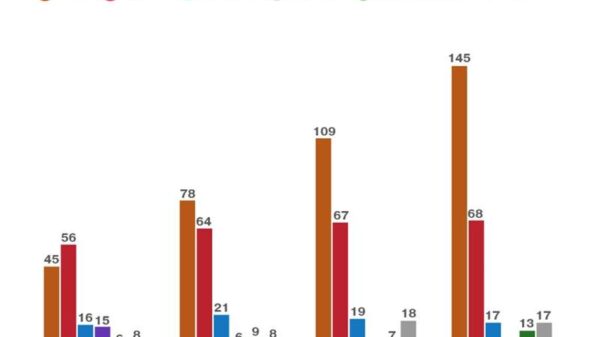
Nationally, the number of people hospitalized with the virus reached 116,000 this week, the most in a year. But a significant number who have tested positive for Covid-19 — anywhere from 20 to 65 percent — were admitted for other reasons and are not primarily ill with virus symptoms, according to hospital officials in many states.
In interviews, nurses and doctors in New York described scenes of distress, including one of a patient urinating in a trash can because she could not get help, and others involving nurses forced to work entire shifts without a break.
Scheena Iyande Tannis, a critical care nurse at Brookdale, said that she and her colleagues had covered additional shifts, “working in waves, as each person is waiting for their turn to get sick.” Still, things seemed better to her than they were in the first virus surge.
“The first time we were just totally decimated,” Ms. Tannis said. “This time, we are overwhelmed but not destroyed.”
New York City is served by a complex ecosystem of about 50 hospitals. The best known are major academic hospitals with imposing Manhattan flagships like NewYork-Presybterian/Weill Cornell and NYU Langone Medical Center.
Then there is the safety-net system, the core of which are the 11 public hospitals run by the city. Augmenting that are about a dozen smaller, independent hospitals that are in working-class neighborhoods outside Manhattan, rely mostly on Medicaid and have been among those hit hardest by the pandemic.
The enormous inequity in the city’s hospitals became clear when the pandemic descended on New York in spring 2020. Safety net hospitals like Brookdale were overwhelmed with patients, but had smaller staffs, worse equipment and less access to drug trials and advanced treatments than their better-financed counterparts.
Dr. Dave A. Chokshi, the city’s health commissioner, said on Thursday that about 80 percent of the hospital beds in the five boroughs were occupied this week, as the number of patients with Covid-19 reached nearly 6,000. That was about half the peak in the first wave, when ballparks and conference centers were turned into field hospitals.
But Dr. Chokshi and hospital executives said the numbers did not tell the full story, as the number of Covid-19 cases continue to climb and because some hospitals do not have enough employees to open all their beds. Isolation requirements for virus patients also mean some beds cannot be used.
“This is why it is so vital for us to surge resources and support to our health care system, particularly to our safety net and H and H hospitals,” Dr. Chokshi said, referring to those run by the city’s hospitals agency. To that end, the city has expanded a loan guarantee program to help hospitals pay for increased staffing while the Omicron wave persists.
Michael Del Valle, a resident physician at Jacobi Medical Center in the Bronx, one of the city-run hospitals, and a vice president of the union that represents residents, said the emergency room there was so crowded that patients had just a foot or two of space between them.
“If you’re in a stretcher, you can touch the person next to you by putting your hand out,” he said.
Dr. Del Valle, who tested positive for the virus this week, estimated that more than 25 percent of Jacobi’s emergency room residents had done the same in recent weeks. With so many patients arriving and so many staff members out sick, it often takes longer than usual for medicine to be administered, he said. Long waits for admission and care have led to angry confrontations.
“There has certainly been an uptick in verbal aggression and physical aggression,” Dr. Del Valle said, adding that Jacobi had added security officers in the emergency room.
The Coronavirus Pandemic: Key Things to Know
The global surge. The coronavirus is spreading faster than ever, but it appears that Omicron is milder than previous variants. Still, the latest surge in cases is causing hospitalizations in the U.S. to rise and lifesaving treatments to be rationed.
Seeking to address the inequities exposed by the pandemic, state officials in December 2020 instituted a system called load balancing for when patient numbers reach critical proportions and hospitals must seek help from one another.
In recent days, Dr. D’Angelo of Northwell said, his system had accepted about a dozen transfer patients from overwhelmed safety net hospitals, including Jamaica Hospital in Queens, an independent hospital where, state data shows, the intensive care unit is full, and the city-run Queens Hospital Center.
Northwell has also agreed to send nurses to Brookdale and Interfaith. Ms. Brown said she was grateful, but that the hospitals needed many more reinforcements.
The loan guarantee program, which Mayor Eric Adams announced on Wednesday, might help pay for expensive travel nurses to fill some of the gaps, she said. Agencies, she added, were now charging up to $215 an hour for critical care nurses.
“We’ll take everything we can get — as my mother would say, beggars can’t be choosers,” said Ms. Brown.
One Brooklyn Health and other hospital systems have also sought help from state officials. Gov. Kathy Hochul, who declared a health care emergency in late November, has authorized nursing students and out-of-state doctors to assist during the current surge. The state has also deployed 120 National Guard members to nursing homes and had directed federal teams to upstate hospitals experiencing their own crises.
The state has not sent staff reinforcements to downstate hospitals, Mr. Raske said.
Jill Montag, a spokeswoman for the state Health Department, did not dispute that, but she said the state was helping hospitals coordinate their efforts and had secured 50 ambulance teams for New York City from the Federal Emergency Management Agency; 25 are to arrive on Saturday.
The problem has been compounded for community hospitals by the way the Omicron wave has spread, starting in wealthier parts of Manhattan and then moving to low-income neighborhoods that rely on safety net hospitals. This week, the Covid positivity rates topped 40 percent in the South Bronx and parts of Brooklyn and Queens. About 37,000 new cases a day are being reported citywide on average.
Longstanding health care disparities mean patients in poor areas are also arriving at hospitals with more pre-existing conditions, and vaccination rates in these areas tend to be lower, contributing to more severe illness. In the Brooklyn ZIP code where Brookdale is, about 2,500 people tested positive for the virus last week, with a positivity rate of 43 percent.
Not all safety net hospitals say they are being stretched to the limit. The area around St. Barnabas Hospital in the Bronx had nearly the highest test positivity rate in the city this week, above 46 percent. But officials said they were dealing with the higher volume, even with 7 to 9 percent of the work force out with Covid-19 or caring for sick relatives.
Not all of the hospital’s intensive care bed are full, and of the 30 patients presently in intensive care at St. Barnabas, only 10 have Covid-19, said Dr. Edward Telzak, the chief of internal medicine. “Covid-19 is not overwhelming us,” he added.
It is different at the pediatric emergency room at Montefiore Hospital, a major nonprofit hospital in the Bronx. Julian Grant, a registered nurse, said the small emergency room was often packed with up to 80 patients, with only two nurses to help them.
More children, she said, were coming in now complaining of difficulty breathing now than had during previous virus waves, although they were usually well enough to be sent home after being given steroids and other treatments. Whether or not they have Covid-19, all of the patients must wait together, raising the specter of the virus spreading to vulnerable children.
“Things have gotten terrible,” she said. “At the end of the day as nurses, it really doesn’t feel good when you can’t take care of your patients.”
Tracey Tully and Joseph Gambardello contributed reporting from New Jersey.