As the Omicron tsunami crashes ashore in New York City, the comforting news that this variant generally causes milder disease overlooks the unfolding tragedy happening on the front lines.
As an emergency room doctor fighting this new surge, I am grateful that vaccines and a potentially less lethal variant have meant that fewer of my patients today need life support than they did at the start of the pandemic. In March 2020, nurses and doctors rushed between patients, endlessly trying to stabilize one before another crashed. Many of my patients needed supplemental oxygen and the sickest needed to be put on ventilators. Many never came off them. Our intensive care units filled beyond capacity, and yet patients kept coming.
Thankfully, this wave is not like that. I haven’t needed to put any Covid-19 patients on a ventilator so far. And the majority of patients haven’t needed supplemental oxygen, either.
We also have good treatment tools: cheap, widely available medications like steroids have proved to be lifesavers for Covid-19 patients. We now know that administering oxygen at high flow rates through the nose substantially improves patient outcomes. Although currently in very short supply, oral antivirals are highly effective at reducing Covid hospitalizations. The greatest relief has come from the vaccines, which keep people out of the hospital regardless of the variant.
Yet these tools are still not enough to slow the rapid influx of patients we’re now seeing from Omicron, and the situation is bleak for health workers and hospitals.
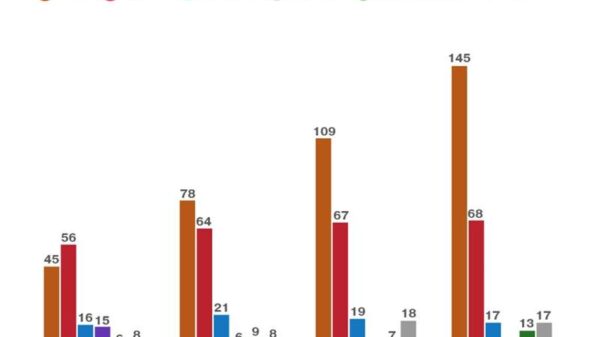
In New York City, hospitalizations have tripled in the past few weeks alone. New Jersey is seeing its highest number of hospitalizations of the whole pandemic. In all, nearly every state and territory is seeing Covid admissions on the rise.
For most people — especially the vaccinated — Omicron presents as a sore throat or a mild inconvenience. But among the many patients in our hospital, the situation is serious. On a recent shift, I still saw “classic” Covid-19 patients, short of breath and needing oxygen. All of them were unvaccinated. I also saw elderly patients for whom Covid rendered them too weak to get out of bed. I treated people with diabetes in whom the virus caused serious and potentially fatal complications.
And even though nearly all of my patients are experiencing milder illness compared with March 2020, they still take up the same amount of space in a hospital bed. Right now, all patients with the coronavirus require isolation, so they don’t infect other patients, and the laborious use of personal protective equipment by health workers. Yes, there’s a fraction of patients who are incidentally found to have the virus — for example, a person needing an appendix removed who tests positive on screening. But entering the hospital with the virus versus for the virus isn’t a relevant distinction if the hospital doesn’t have the beds or providers needed to care for its patients.
This influx of coronavirus-positive patients is also creating another source of infection for health care workers, who are being sidelined in numbers I’ve never seen before. In March 2020, we clamored for critical supplies like masks and gowns. When patients piled up, we built makeshift treatment centers in tents, sports stadiums and floating ships. What’s in critically short supply now is health care providers, and qualified staff members are significantly harder to scale up than supplies or space.
Thankfully, nearly all my colleagues on the front line are now vaccinated, so I am not worried that I will see them coming into the E.R. as patients or dying, as some did in 2020. But many hospitals are seeing their highest levels of employee infections of the pandemic. Some hospitals in the United States have lost 15 percent of their work force or more.
When a health care worker falls ill, another steps in to cover the shifts. But there are only so many of us. Updated guidance from the Centers for Disease Control and Prevention that shortens isolation time after testing positive for the virus allows health care workers to return to work earlier. This may help. But in some places, like Rhode Island and California, severe staffing shortages have led to contingency plans that allow providers still testing positive to return to work. Sending potentially contagious nurses or doctors to treat patients seems inconsistent with the principle of “first, do no harm.” But the alternative is that patients wait longer for care, or worse, there isn’t a provider to care for them at all. These are awful decisions to make two years into the pandemic.
The harsh reality is this: Fewer providers means fewer available beds because there are only so many patients a team can treat at a time. This also means treatment is slower and people will spend more time in the E.R. And the longer these patients stay in the E.R., the longer others remain in the waiting room. The domino effect will affect all levels of the health care system, from short-staffed nursing homes to ambulances taking longer to respond to 911 calls.
It’s understandable that people are tired of Covid-19. Health workers are, too. But leaning too heavily on us and our hospital beds is foolhardy. A highly contagious variant like Omicron, even if it causes milder illness, can still risk precipitating the failure of our health care system. Collective actions over the coming weeks — the distribution and use of high-quality masks, staying home if not feeling well and getting vaccinated or a booster if eligible — could help prevent hospitals and health care workers from sliding into crisis. It’s not March 2020. But it shouldn’t have to be for us to take this seriously.
Craig Spencer (@Craig_A_Spencer) is an emergency medicine physician and director of global health in emergency medicine at NewYork-Presbyterian/Columbia University Irving Medical Center.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips. And here’s our email: letters@nytimes.com.
Follow The New York Times Opinion section on Facebook, Twitter (@NYTopinion) and Instagram.