With Covid surging again and vaccine fatigue rising, vaccination rates for influenza are troublingly low, especially among older Americans.
Jillian Gibson hasn’t gotten a flu shot in some 25 years.
“I don’t get the flu, and I’ve been exposed over and over,” said Ms. Gibson, 75, a mostly retired office manager for a medical practice in Beverly Hills.
True, she endured one bout back in the ’80s — “I remember being dreadfully sick” — and had a head cold a few years ago. Otherwise, despite urging by virtually every public health authority that seniors (and everyone else over six months old) be vaccinated against influenza annually, “I just didn’t do it because I don’t get sick,” she said.
Ms. Gibson doesn’t mistrust vaccines in general, she added. Her three children were always up-to-date on immunizations, and she herself got flu shots decades ago when she worked with dementia patients at an adult day center.
Now she doesn’t, even though she is more vulnerable to illness after two recent heart attacks.
People like Ms. Gibson make physicians like Dr. William Schaffner very uneasy, especially this year. “The preoccupation with Covid and a certain vaccine fatigue mean that people need to be reminded about flu,” said Dr. Schaffner, an infectious disease specialist at the Vanderbilt University School of Medicine.
Americans tend to sound cavalier about flu; falsely comparing Covid-19 to flu was a way of dismissing the new virus as no big deal. But deaths from influenza range from 12,000 nationally in an unusually mild year to 60,000 or more in a virulent one. An estimated 75 to 80 percent of flu-related deaths occur in people over 65, principally from pneumonia.
Flu also sends hundreds of thousands of Americans to the hospital annually, and evidence is emerging of its association with other serious diseases.
Yet vaccination among older Americans, those most apt to accumulate the chronic conditions that can make flu particularly dangerous, has remained stuck at roughly 65 percent in most recent years, leaving millions unprotected.
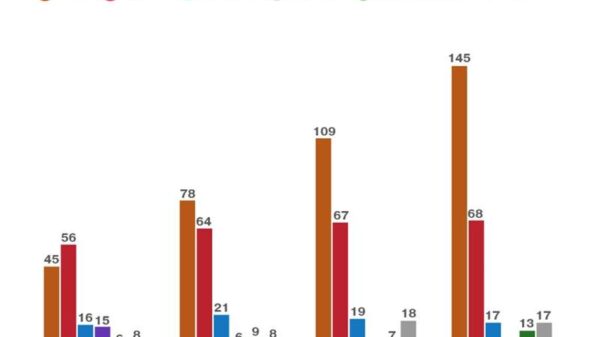
This year, based on early reporting, the rate appears to be even lower. In October 2019, almost 20 percent of Medicare fee-for-service beneficiaries had already been vaccinated, according to the Centers for Disease Control and Prevention; in October 2020, the proportion reached close to 30 percent.
This past October, only 11 percent of seniors had received a shot.
“I think it’s going to be a bad flu year,” said Nathaniel Hupert, a co-director of the Cornell Institute for Disease and Disaster Preparedness. “The trajectory is just like prior bad flu years — 2017, 2019. And for reasons that are unclear, we have this incredibly low rate of vaccination reported among older people.”
This season’s dominant H3N2 strain, he added, poses “a particular threat to older people,” although existing antiviral medications appear effective against it.
Perhaps people grew complacent because last season, despite fears of a “twindemic” that would simultaneously hospitalize both flu and Covid-19 patients, flu infections actually plummeted. “The lowest season ever,” Dr. Schaffner said.
Last winter “we were all at home, all wearing masks,” Dr. Schaffner said. “Children play a major role in spreading the flu, and last year they were all learning remotely. Now, all of that is reversed” — and the C.D.C. reports that outpatient visits for flulike illnesses are climbing sharply, especially in the East and Midwest.
Even if the flu season turns out to be moderate, with returns to school, work and travel, and with the rampaging Omicron variant, this could be the year that both flu and Covid patients swamp struggling hospitals and health systems.
Moreover, researchers are reporting that flu can lead to other health crises, especially in older patients. In 2018, Canadian researchers found a link to heart attacks, for instance.
Using data from Ontario residents (average age 77) who had influenza, “your risk of having a heart attack is six times higher during the seven days after testing positive” than in the year before or afterward, said Jeffrey Kwong, a senior scientist at ICES, a nonprofit research institute in Toronto. Other studies have found similar results.
The cause might be increased stress on the heart from a fever, Dr. Kwong noted; respiratory viruses can also create inflammation. In either case, “the influenza vaccine can actually decrease the risk of hospitalization and death from heart attacks,” he said.
A new study in JAMA Neurology, drawn from Danish health records, also found an association between influenza and an increased risk of developing Parkinson’s disease a decade or more later.
The Coronavirus Pandemic: Key Things to Know
The latest Covid data in the U.S. As the Omicron surge causes case counts to reach record highs and hospitalizations to surpass the height of the Delta wave, here’s how to think about the data and what it’s beginning to show about Omicron’s potential toll across the county.
Given such prospects, what makes vaccinating more older adults such a challenge? Improvement appears possible. The C.D.C. has reported that last year — when public health strategies emphasized flattening the hospitalization curve, protecting essential workers and preserving resources for Covid patients — the proportion of older people who were vaccinated against flu rose 9.5 percent in selected jurisdictions.
Further, a new C.D.C. study has found that three-quarters of unvaccinated Medicare beneficiaries actually visit a health care provider during flu season, with even more such “missed opportunities” among Black and Hispanic beneficiaries.
Nevertheless, in most years, one-third of older people, like Ms. Gibson, shrug off vaccination. They may figure that a shot that is 40 to 60 percent effective (scientists must reformulate it each year as new flu strains circulate) won’t make much difference.
But even if people contract the flu, the shot substantially reduces the risk of severe illness and hospitalization. “Why would someone turn down a 50 percent chance of avoiding a serious illness?” Dr. Hupert said.
Older patients also may not be hearing strong enough recommendations from their health care providers. Many patients rely primarily on specialists — endocrinologists, oncologists, nephrologists — who are not trained in routine care and don’t typically stock flu vaccines in their offices, Dr. Schaffner said.
That puts a lot of the responsibility on older people to seek out shots. It is not too late to be vaccinated against flu, although people should not delay, because it takes 10 to 14 days for full immunization to develop. “Classically, February and early March is when flu is most prominent in the U.S.,” Dr. Schaffner said.
Patients can receive flu vaccines and Covid shots and boosters at the same time — and they need both, because neither provides protection against the other disease. Two flu vaccines designed especially for the older population, Fluzone High-Dose and Fluad Quadrivalent, generate stronger immune responses.
Dr. Schaffner has found that some of his patients are understandably weary of the whole subject: “They say, ‘You’re telling me I have to get another vaccine?’” His response, for their own health and for the sake of an already stressed health care system, is yes. Yes, they do.