A new book offers guidance on how family members can support a critically ill loved one who ends up in the hospital’s intensive care unit.
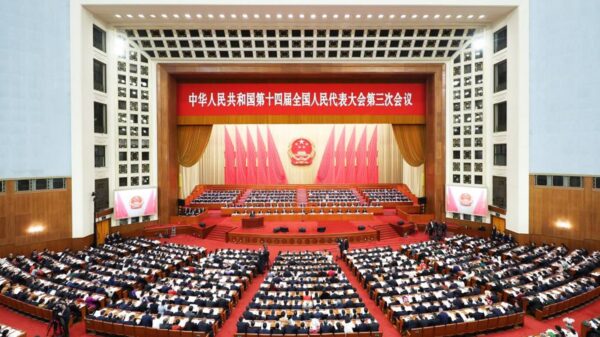
In the last two years, the letters I.C.U. have become almost as familiar to the listening and reading public as PBS and NBC, as intensive care units across the country have been overwhelmed with people suffering from severe Covid-19. Meanwhile, medical personnel continue to struggle to care for patients with serious injuries, diseases or surgical complications who also require critical care.
Intensive care can be a difficult and traumatizing experience for patients whose lives depend on it. And, according to the author of an extraordinarily thorough and helpful new book, the families and friends of patients who require prolonged stays in an I.C.U. often suffer along with them. Their fears skyrocket and unanswered questions abound. What is happening to my loved one? What are all these tubes, machines, flashing lights and warning bells? Who is in charge here? Whom can I talk to?
In her new book, “The I.C.U. Guide for Families: Understanding Intensive Care and How You Can Support Your Loved One,” Dr. Lara Goitein, who spent 12 years as an intensive care physician, provides comprehensive yet easy-to-understand answers to myriad questions like these and many others you might not think to ask. Ideally, families would have this book at the ready when needed, like a first-aid manual, because the initial days in an I.C.U. are often the most stressful and disconcerting.
“It helps to be educated and know how you can contribute,” said Dr. Goitein, a pulmonary and critical care physician in Santa Fe. The goal, she said, is to assure the best possible outcome for patients and their loved ones, all of whom can experience a version of post-traumatic stress disorder following a long stay in an I.C.U.
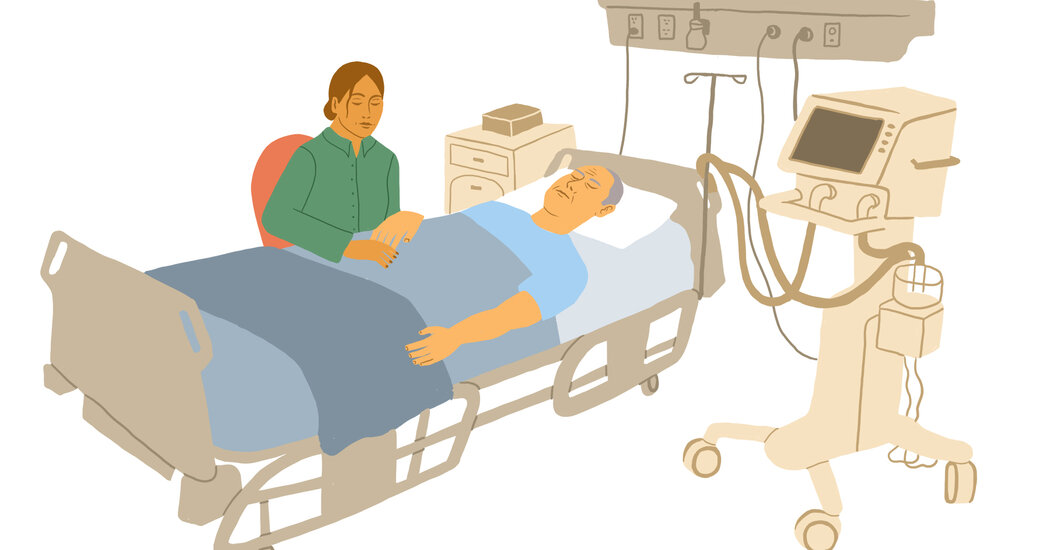
Juli Barde of Portland, Ore., whose husband Rick, then 59, was in an I.C.U. for six weeks early in the pandemic with near-fatal Covid, said she stayed with him for four or five hours every day to provide comfort and be his advocate. “I watched carefully and learned a lot,” Ms. Barde told me. “With three tubes in his trachea, he couldn’t speak for himself, so I had to speak for him. I can read his facial expressions and knew what was going to bother him.” And when careless nursing care led to a serious complication, Ms. Barde was there to call for a replacement nurse and report the incident to a supervisor.
Of course, few families can spend half their waking hours in an I.C.U. But by understanding what is happening, recognizing the signs of improvement and deterioration in a patient’s condition and knowing when it’s appropriate to intervene on the patient’s behalf can result in better care all around. That’s what makes Dr. Goitein’s book so valuable and destined to remain on my bookshelf until my dying day.
The ability to hope for the best but prepare for the worst is likely the biggest challenge families face when a loved one is in an I.C.U. with a condition from which recovery is uncertain. Although 80 to 90 percent of I.C.U. patients — many of whom are very sick — are eventually able to transfer out of intensive care and leave the hospital, families need a realistic picture of what survival will be like.
For patients who were treated in an I.C.U., Dr. Goitein said, “many improve over the first year, and some need help for symptoms that persist for a year or longer. But most of those who make it through that first year, by three years they are independent.”
Patients’ future prospects depend greatly on the reason they required I.C.U. care in the first place, as well as their age, prior physical condition, emotional health and resilience and their ability to pursue needed rehabilitation. Among those who required prolonged life support, only a minority go directly home after being discharged from the hospital, Dr. Goitein reported. A fifth are transferred to an inpatient rehabilitation facility, another fifth go to a skilled nursing facility and more than a third require long-term acute care.
“Most people focus on very small hopes, and they expect the patient to survive, go home and be the same person he was before,” Dr. Goitein said. “But a long, difficult battle with illness can result in psychiatric as well as physical disability. It’s more stressful than people estimate.”
For patients who needed more than two days of mechanical ventilation in the I.C.U., family caregivers typically spend an average of more than five hours a day giving care during the first half-year after hospital discharge, she said. How well the family copes often depends on how carefully they plan and prepare before the patient comes home. Are there grab bars in the bathroom? Will a walker or wheelchair fit through doorways? Can the patient communicate readily with the caregiver?
After a long stay in an I.C.U., it’s not uncommon for patients to experience what doctors call “post-intensive care syndrome,” or PICS. “Overall, about half of survivors will have at least one cognitive, psychiatric or physical problem that persists for weeks, months or even years after discharge,” Dr. Goitein wrote. These may include problems with memory, concentration and problem-solving. Emotional consequences like depression, anxiety, post-traumatic stress disorder and sleep disturbances sometimes persist for years. Overcoming I.C.U.-induced physical weakness can take several years, and regaining independence in activities of daily living, like getting dressed and preparing meals, can require fierce determination and infinite patience on the part of both patient and caregiver.
An excellent resource for patients and their families following I.C.U. care is Thrive, an online initiative of the Society for Critical Care Medicine. The site maintains a partial list of clinics that provide specialized care for patients after an I.C.U. stay.
It’s also important for families to know when “enough is enough,” Dr. Goitein said. For patients who’ve been on prolonged life support in the I.C.U., it can be very challenging for families to come to terms with their failure to improve and inability to wean them off the machines keeping them technically alive.
Ideally, well before a life-threatening crisis, patients will have completed an advance directive and assigned a trusted health care proxy or agent, who has a clear understanding of their wishes and can speak for them when they cannot speak for themselves. What are the patients’ values? What makes their life meaningful? What level of disability would they consider intolerable?
The proxy’s job, Dr. Goitein said, “is to put their own desires and beliefs aside and choose what the patient would have wanted for himself,” in effect respecting the autonomy of a terminally ill person who is no longer able to communicate their wishes. When family members disagree, she said, discussion with the doctor in charge may facilitate a decision.